Case #8 Reducing Hba1c, without drastically changing diet or lifestyle🗒️
By nutritionists from Hugg (gethugg.com)
Client Presentation
Neha ji [name changed], a 62-year old female, came to us with one objective: she wanted to reduce her blood sugar.
She had been a diabetic for nearly 14 years, but during COVID her Hba1c had shot up to nearly 10%.
This made her feet ‘tingle’ - a very common symptom for many diabetics.
She was not taking any allopathic medicine or insulin; she was keen to reduce her blood sugar naturally.
Based on what she read about and learned online, she had already:
Replaced 70% of grains with millets
Started intermittent fasting (skipping breakfast)
Started high intensity yoga 3 times a week
Drastically reduced her meal portion sizes
Still, her blood sugar had NOT budged from the 10% mark.
She regularly ate non vegetarian food, and had the occassional alcoholic drink during social settings.
Finding the root cause
With her permission, we attached a continuous glucose monitor (FreeStyle Libre Pro) on her arm.
This is a small sensor which automatically captures a blood sugar reading every 15 minutes.
This gives 96 readings in a day; enough for us to paint a comprehensive picture of what was going wrong.
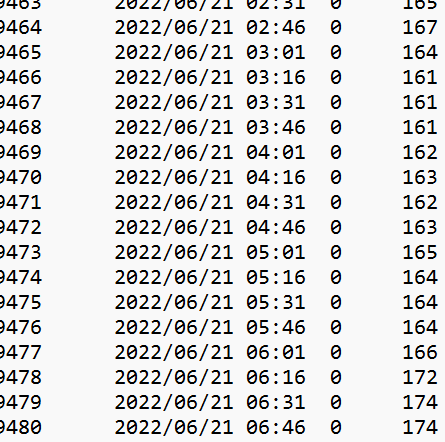
The reader shares results in this format:
If you take the average of all the readings for one day, you get the estimated average glucose (EAG).
Based on conversion tables published by the American Diabetes Association, you can convert the EAG to HBa1c.
We checked her average on the first day to check if the CGM was properly calibrated.
The average of all the readings on the first day was 228mg/DL.
An average of 228mg/DL converts into an Hba1c of 9.6%.
This matches closely with a report we did barely 2 weeks ago.
This confirmed that the CGM was working properly.
Second, we converted the readings into graphs to evaluate them better.
Here is an example of one full day.
Here is what she ate throughout the day.
Remember, because of her intermittent fasting routine, her first meal is at 12 PM (lunch), and last meal is at 8:30 PM.
Salad, fish and millets increasing blood sugar by nearly 100 points?
A few banana wafers causing a spike from 170 to 270?
A salad, half katori chana and a mango pushing blood sugar into the 300s?
This data was very surprising!
Here are some more of her meals during the week.
You’ll notice:
Portions are very tiny. She barely eats!
Several veggies, usually in 50:50 proportion to anything else.
There is a focus on protein, too.
Now, compare these to her readings throughout the week.
You’ll notice that her blood sugar almost NEVER leaves the yellow band of 200 and 300.
It’s almost as if her body is operating at a new normal. For most people, this is between 100 and 140 mg/DL.
For Neha ji, it had become 200 to 300 mg/DL.
Of course, there were changes we could have made to her meals.
But when the body has become this sensitive to even small quantities of food, we’ve found it best to look elsewhere.
We hypothesized that the problem wasn’t her diet and took another look at her blood report, and specifically her lipid profile.
Her triglycerides were uncharacteristally high for someone with her diet! They should usually be under 150. Even her LDL was higher than normal.
This clearly indicated slow liver function - the chief organ when it comes to lipid management.
This also indicated that her ‘occassional drink’ was more frequent than it seemed.
When we confronted her about his, we learned that during COVID, a 30ml drink had almost become a daily activity.
30ml of alcohol a day for a prolonged period of time is enough to form a fatty liver.
With a fatty liver, some hepatic cells are replaced by adipose cells and the liver loses its ability to regular the storage and release of glycogen as effectively.
This leads to highly sensitive blood sugar control. In fact, nearly 40% of diabetics have a fatty or slow liver and are called diabetic dyslipidemics.
With this, we decided to target her liver health in particular.
We offered her the Mango Leaf Tonic, a morning juice made with Mango leaves, Kalmegh leaves, Moringa leaves and a range of other spices specifically designed for diabetic dyslipidemics.
It is made with 100% real ingredients (read: whole leaves), so we opted for this versus a churan or tablet made with processed extracts.
The recommendation was simple: for one week just drink the Mango Leaf tonic on an empty stomach in the the morning.
Here is what happened:
By day 2, her blood sugar was already moving towards the 150 mark! It was below the yellow range of 200-300 for nearly the entire day.
Unlike juices like Jamun Karela or Methi paani which usually show a result for a few hours, this juice was addressing the root cause (Neha ji’s liver) and helping to keep the blood sugar underneath the yellow bar for the ENTIRE day.
Fasting blood glucose had dropped into the 170s versus the usual 200mg/DL.
Spikes post meals were also halved, increasing by only 50-70 points versus the usual 100.
In fact, for the first time in 3 years, her readings actually went as low as 138mg/DL.
This is all within 48 hours of starting the tonic.
On average, her blood sugar fell from 220 to 180mg/DL.
In Hba1c terms, that is a decrease from 9.6% to nearly 8%, without changing ANYTHING in her diet.
Recommendation #1: Continue Tonic for 3 months.
But the work wasn’t finished. We noticed that for faster recovery, it was vital for her alcohol to stop completely.
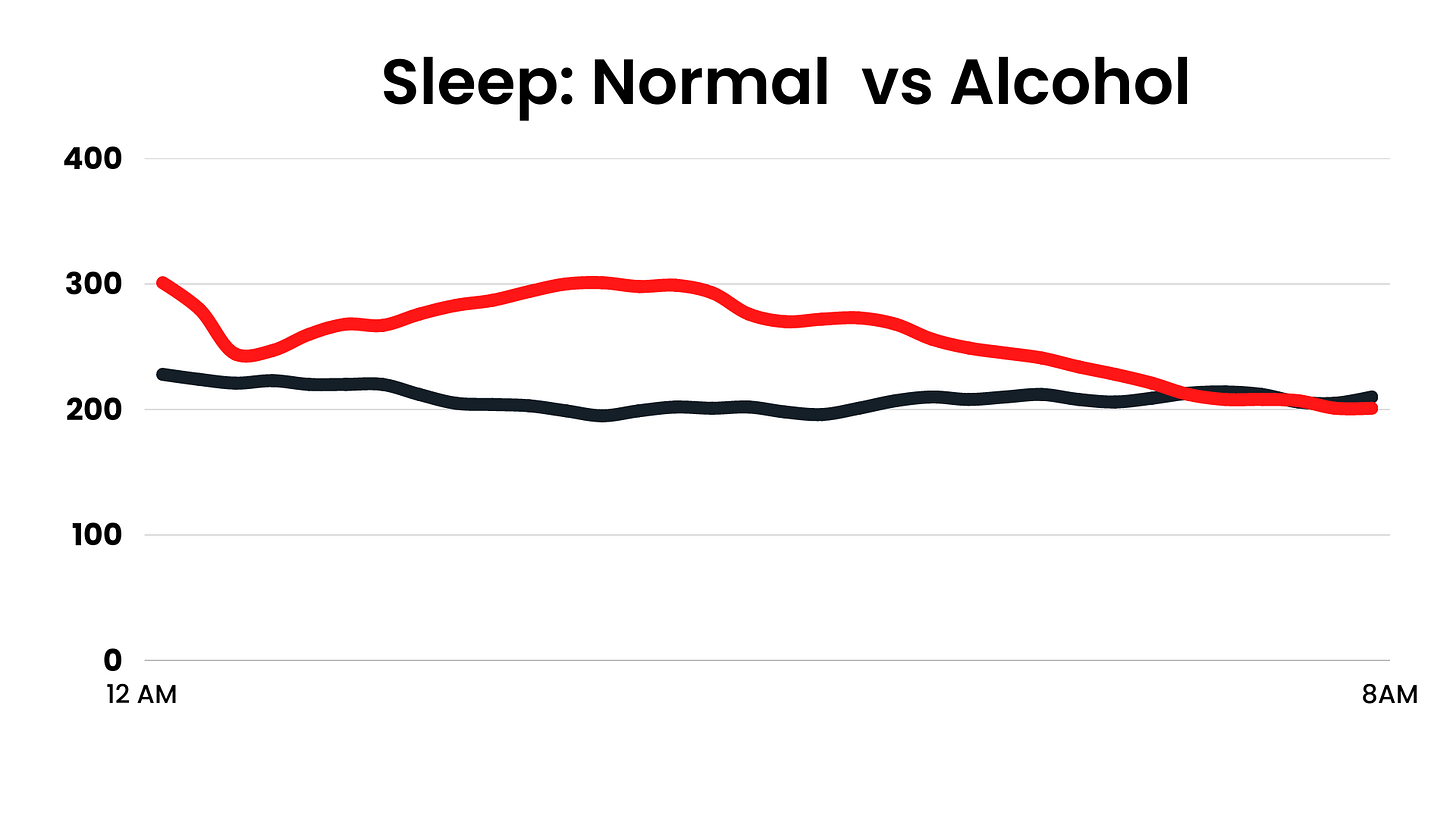
Take a look at what a single drink does to her sleep for 8 hours, for example.
The line in red is what happens after she drinks alcohol.
The line in black is what happens on a normal night.
Readings are increased by nearly 100 points for 4-5 hours!
The line in green shows what happens on a night she drinks the tonic, but doesn’t drink alcohol.
Recommendation #2: Stop Alcohol.
Exercise plays a huge role in liver recovery.
Her walking and yoga classes reflected this.
Take a look at how physical activity improved her blood glucose management.
Difference of 30 to 70 points in a matter of one hour is quite extraordinary!
We recommended she increase her frequency, and either go for a walk or do yoga daily.
Recommendation #3: Walk or yoga, daily.
We also evaluated her eating patterns.
On the days that she ate carbs after a Yoga class (June 15 and June 17, for example), blood sugar nearly doubled.
On the days she went for a walk after eating (June 18, for example) or just drank coffee (June 22, for example) blood sugar fell.
So we recommended that she reduce her snacking frequency to once in two days, and/or go for a walk after she had a snack.
This would take care of the post-snack spike that is very common across her graphs.
Recommendation #4: Walk after snacking.
We additionally offered some small dietary pointers: lighter meals and soups at night, and some dried fruit alongside fruits to better manage her glycemic load.
1-Week Follow Up
Neha ji’s tingling-in-feet has almost entirely stopped - a direct result of blood sugar decreasing.
She is rigorously adhering to the changes we’ve recommended. As it is, we expect her Hba1c to drop to 8% with just recommendation # 1 (drink juice) and #2 (abstain from alcohol).
We additionally expect her Hba1c to fall into the mid-to-high sixes with recommendation #3 (physical activity daily) and #4 (walk after snacking, minor dietary modifications).
We will publish another update to her blood reports one more time once we receive them by the end of August.
Know someone in Mumbai who is struggling with blood sugar and fatty liver like Neha ji? Just write to me on harsh.doshi@hatabevtech.com, and we’ll set up a CGM for them :)
Want to know more about the Mango Leaf Tonic for your own practice or use? Just write to me on harsh.doshi@hatabevtech.com, and I’ll guide you further.














Great case and learnings. Is Mango leaf tonic advisable for Gestational diabetes??
may I know the amount you prescribed the tonic to individual